The real threat to gender-diverse children is the politicization of care issues like puberty blockers and detransition
Under the pretext of protecting children, Pierre Poilievre, leader of the Conservative Party of Canada, has said he is opposed to the use of puberty blockers for gender-diverse children.
“I think that we should protect children and their ability to make adult decisions when they’re adults,” Poilievre said.
Poilievre is one among many politicians to wade into debates surrounding gender-affirming health care in recent years. Alberta Premier Danielle Smith has proposed controversial policies that would affect gender-diverse youth, including prohibiting puberty blockers for children aged 15 and under.
But the growth of politicization and misinformation on this issue — on top of already longstanding ideological battles over the care of minors — probably pose a bigger threat to gender-diverse people than puberty blockers.
We are researchers who study the experiences of transgender and gender-diverse people who have accessed gender-affirming health care. One of us is transgender and also a parent. And we are among a few who also research detransitioning — the process of discontinuing or reversing a gender transition.
We both personally know countless people who have been helped by transitioning, as well as others who were let down by the promises of gender-related treatments that can have life-altering consequences.
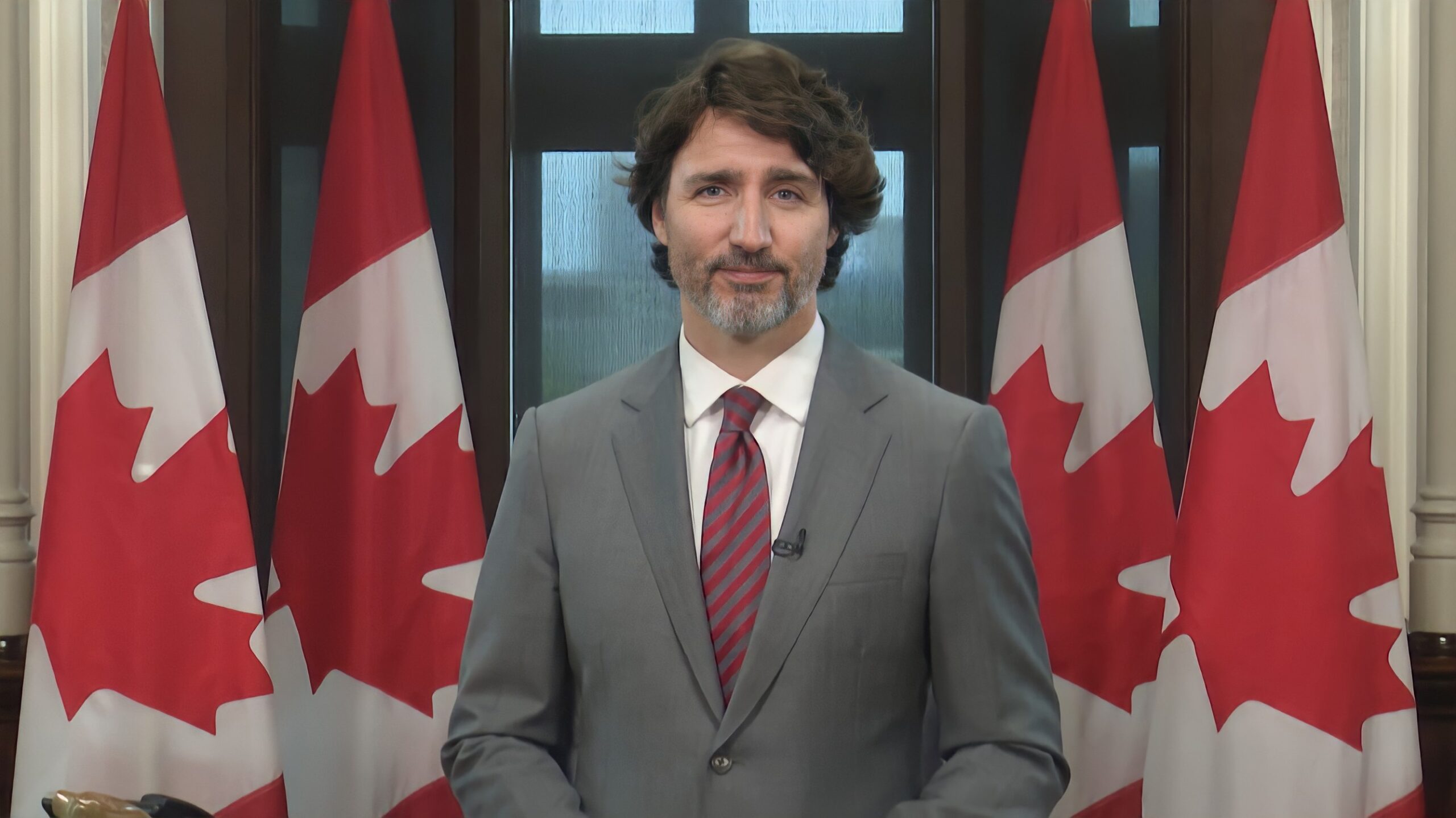
We have noticed that what is presented as “fact” in these debates has distorted real complexities of gender-affirming health care, creating a rift between conservative and progressive information outlets. The result has left many in the dark about what is really at stake. Conservative leader Pierre Poilievre speaks to the media about puberty blockers and trans children.
Fertility and gender-affirming medicine
Take the New York Times as an example. Two opinion columnists recently wrote about gender-affirming care for minors, making drastically different remarks about the fertility implications of this care.
Opinion columnist Lydia Polgreen asserted that it is a “mistaken belief” that infertility routinely results from treatments for gender-diverse children, while Pamela Paul, writing about detransition, claimed that hormonal therapy causes “often irreversible” infertility.
But the reality of fertility and gender-affirming treatments is in the details. Research on fertility outcomes is lackluster to begin with, but outcomes are highly sensitive to whether puberty blockers were taken prior to starting cross-sex hormones and the stage of puberty.
For children who start puberty blockers followed by cross-sex hormones without ever undergoing natal puberty, infertility is presumed because reproductive maturity is not achieved, and saving sperm or eggs for the future is not possible with current assisted reproductive technologies. However, for transgender people who begin cross-sex hormones after undergoing at least some natal puberty, fertility does not seem to be permanently affected.
Early research indicates that for those who went through natal puberty, taking cross-sex hormones alone is unlikely to cause permanent sterility.
Puberty blockers
The history of transgender medicine and reproductive rights has been fraught with injustice. When puberty blockers were first tested for use with gender dysphoric youth, transgender adults were being coercively sterilized. In 2014, the Netherlands struck down a policy requiring sterilizing surgeries to legally change genders and paid out financial reparations as an apology.
Pediatric gender medicine is a relatively new field, and while the evidence base is growing steadily it also shows its novelty.
In fact, fertility is not the only issue at stake with puberty blockers. There are uncertain impacts on bone health, neurodevelopment and social development, as well as sexual function — issues clinicians and researchers are paying close attention to.
A team of Dutch clinicians who were among the first to offer transgender children puberty blockers recently acknowledged that these drugs may not be just a “pause button” to explore identity, as originally intended. Instead, they should be thought of as the first step of a medical gender transition, because a majority eventually go on to take hormonal treatments.
But there are also major consequences involved in delaying or withholding treatment with puberty blockers, which could hurt transgender girls more than boys. Testosterone’s effects on the body can be difficult to reverse, so undergoing a masculinizing puberty could render transfeminine kids more vulnerable to future anti-trans discrimination. Irreversible body changes from puberty can not only heighten distress and reduce social acceptance, but also contribute to a need for future surgeries.
Given that puberty may occur as early as eight or nine years old for some children, this is a high-stakes medical decision never taken lightly by families or clinicians. Poilievre gives the wrong impression by saying that “we should protect the rights of parents to make their own decision with regards to their children,” because, given the age of the child, parents are typically involved in the decision to start puberty blockers.
However, there is always some risk of getting it wrong — in either direction.
Detransition debate
Puberty-blocking drugs are not the only politicized topic in gender-affirming health care. Detransition also tops the list.
On one side, opponents of gender-affirming care distort studies to argue detransition has reached epidemic proportions and draw from testimonies of regretful detransitioners as a “cautionary tale against medical transitioning.”
Proponents retort by dismissing detransition either by alluding to its “rarity,” using outdated and flawed studies, or by decoupling the experience from regret.
As a result, the public is exposed to two different sets of “facts,” none of which reflect the heterogeneity that we and others have encountered in researching detransition — different psychological, medical and social motives for detransitioning; a range of emotions including regret, resilience, and satisfaction; expansive patterns of identity discovery and fluidity. All of it must be studied for gender-related medical care to continue being evidence-informed.
But threats, or outright restrictions, from politicians will not advance this care. What is badly needed from governments is investments in higher quality research and systems of care so treatments can be accessed in the safest possible terms. There are currently gaps in the Canadian gender-affirming care system affecting access, quality, and safety.
Guidelines, dilemmas and the need for high-quality research
This area of health care already has guidelines developed through a review of the evidence and international expert consensus. But that does not mean the science is settled or that the medicine has no room for improvement.
Gender-affirming care is riddled with ethical dilemmas that have spilled over into an explosive political situation. The changing landscape of transgender health care, debates about puberty blockers and detransition are all low-hanging fruit for opportunistic politicians like Poilievre.
On the polarization of these topics, anthropologist and medical doctor Sahar Sadjadi — who studied in-depth some of the first American pediatric gender clinics — wrote:
“It is tempting to take the opposite position of one’s enemy, by defending all medical interventions currently associated with gender transition in children and insisting that they are safe and save children’s lives.”
But by not being able to tolerate some of the unknowns, or banning treatments outright, we miss a crucial opportunity to advance knowledge that is needed to help gender-diverse children and their families.
Debate should not centre on whether to ban blockers, but on how to build a high-quality health and social care system that can support all gender-diverse people. Doing so depends on our collective ability to tolerate complexity.
As published in the Conversation Canada