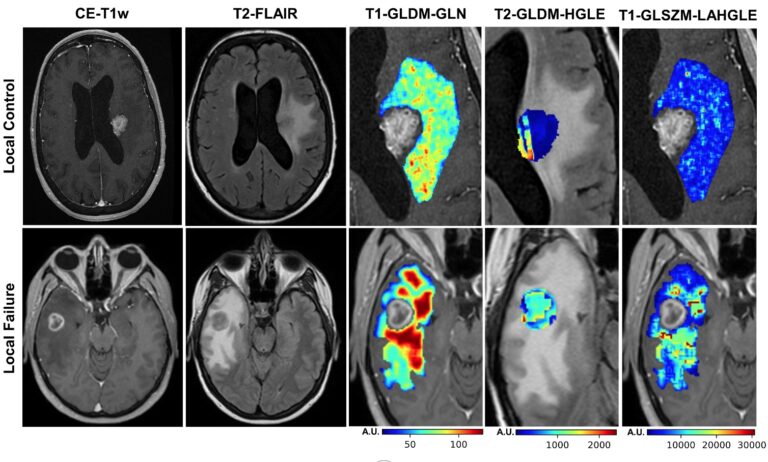
The quantitative MRI biomarker developed in this project can predict whether a patient’s tumor is likely to be controlled by stereotactic radiotherapy (SRT) or if the treatment is likely to fail.
Predicting the success of cancer treatment strategies is paramount for clinicians to provide the highest standard of care to patients. While predicting these treatment outcomes is a difficult science, Lassonde School of Engineering Professor Ali Sadeghi-Naini has been making significant progress in doing just that.
Sadeghi-Naini, an associate professor in the Electrical Engineering and Computer Science department and York Research Chair in Quantitative Imaging and Smart Biomarkers, has been working in concert with clinicians from Sunnybrook Hospital to improve the standard of care for cancer patients.
Brain metastases, a cancer in the brain resulting from a primary cancer in another part of the body that has spread, represent an underdeveloped yet critical area in cancer treatment. While whole brain radiation therapy (WBRT) is a treatment option, it is associated with negative side effects such as cognitive dysfunction. This is what has triggered a paradigm shift in radiotherapy, moving towards more precise irradiation of tumors known as stereotactic radiotherapy (SRT).
A recently published study in Nature Scientific Reports entitled, “A priori prediction of local failure in brain metastasis after hypo-fractionated stereotactic radiotherapy using quantitative MRI and machine learning” by Sadeghi-Naini and his team has outlined a methodology to predict how patients will respond to SRT based off of standard-of-care imaging. Clinicians can use this information, at pre-treatment, to facilitate the best plan for patients.
Using quantitative magnetic resonance imaging (MRI), Sadeghi-Naini’s team can predict whether a patient’s tumor is likely to be controlled by SRT or if the treatment is likely to fail.

“All patients undergo MRI and CT as part of their standard-of-care treatment planning,” explained Sadeghi-Naini. “Therefore, this method has the benefit of not requiring anything additional from the patient side, but it has the potential to improve their treatment plan.”
These images are acquired prior to the treatment and, through quantitative analysis, the morphology and heterogeneity of the tumor can be characterized. Specifically, Sadeghi-Naini is concerned with quantifying the heterogeneity within the tumor site and its surroundings as these varied features are shown to strongly correlate with treatment outcomes. His machine learning (ML) models have demonstrated improved accuracy and sensitivity compared to existing methods.
Current medical practice for evaluating treatment outcomes revolve around clinical follow-ups post-treatment, but if the treatment is not successful, as it is for at least 20 per cent of all patients, this process poses a major issue. With clinicians knowing the likelihood of treatment success in advance, they can make more informed decisions and potentially improve the rate of successful outcomes for patients.
“The features identified with machine learning (ML) algorithms are not easily interpreted by clinicians and, at a glance, individuals can only describe them in terms of heterogeneity,” said Sadeghi-Naini. “Using ML, we can differentiate these features and create a model with statistics that we can provide to clinicians to enable them to make the most informed decision possible.”
Going forward, Sadeghi-Naini is aiming to acquire data from larger cohorts of patients to further optimize and validate these methods. While his model is already a major improvement from existing methods of prediction, his team is investigating other ML solutions such as deep learning approaches to enhance the model.
Working within this interdisciplinary field is a long journey of practice, as the jargon and terminology varies drastically between medicine, engineering and computer science. Sadeghi-Naini has worked with clinicians for years and currently holds a cross appointment as a scientist at Sunnybrook Hospital. The willingness of his collaborating clinicians to work closely with him has allowed students from Sadeghi-Naini’s team to gain unique experiences working with clinicians and in clinical environments.
“My students have the opportunity to spend time regularly at [Sunnybrook] hospital, acquiring the data, observing the processes and working directly with clinicians,” said Sadeghi-Naini. “These worlds of engineering and medicine are very different, so this is a great opportunity for students to see how interdisciplinary projects are run and learn from both perspectives.”
To learn more about Research & Innovation at York: follow us at @YUResearch; watch the animated video which profiles current research strengths and areas of opportunity, such as artificial intelligence and Indigenous futurities; and see the snapshot infographic, a glimpse of the year’s successes.
