
By Ashley Goodfellow Craig, YFile editor
York University Assistant Professor Ian Stedman says the diagnosis of his first-born daughter’s rare disease likely saved his life – and now, he’s focusing his work on helping to do the same for others across Canada.

The Osgoode Hall Law School alum and lawyer – appointed as assistant professor in the School of Public Policy & Administration in the Faculty of Liberal Arts & Professional Studies, with graduate appointments at Osgoode, in Science and Technology Studies and in Socio-Legal Studies – is a co-applicant on a $15-million project that aims to disrupt the current health-care model through the development of a first-of-its-kind national genomics database.
The Pan-Canadian Human Genome Library (PCHGL), funded through a five-year grant from the Canadian Institutes of Health Research, will bring together human genome sequencing initiatives across the nation to enhance the collective well-being of people in Canada.
It will have huge implications for health care, says Stedman, especially for those living with rare diseases and struggling to find a diagnosis – an experience he’s lived through.
Beginning at a young age, Stedman suffered from a host of symptoms that grew in severity as he got older – frequent rashes, periodic fevers, headaches, bloodshot eyes, arthritis and eventually hearing loss – that had doctors and specialists stumped for more than 30 years.
Looking back over his health records from the first 18 years of his life, Stedman noted 190 separate visits to his family doctor, walk-in clinics and specialists – not to mention the many visits to emergency departments when his pain became unbearable – that had him seeking answers to his ongoing progressive illness.
“So, my story is 30 years undiagnosed, having no idea what was going on, and then just giving up,” says Stedman.
That was, until his daughter Lia began exhibiting similar symptoms during her first year of life. When her health declined a few months before her first birthday, she was brought to the SickKids emergency room, which marked the beginning of their diagnostic journey together.

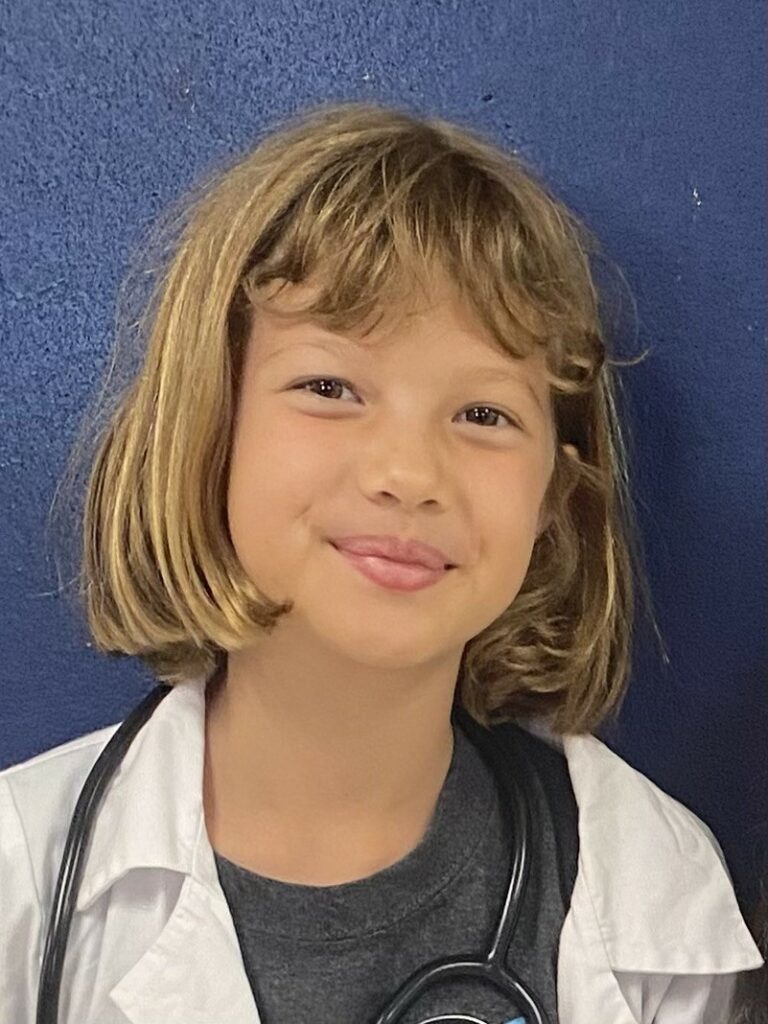
In 2014, both father and daughter were diagnosed with a one-in-a-million genetic disorder called Muckle-Wells syndrome (MWS), a member of the family of genetic disorders known as cryopyrin associated periodic syndromes. Thought to be the 12th and 13th in Canada to receive the diagnosis – with the confirmation of Lia’s MWS leading to his same diagnosis – Stedman learned that if left untreated, the syndrome results in premature death before the age of 36 for one in three people.
He was 32.
After diagnosis, and with the realization that his daughter had potentially saved his life, Stedman began his advocacy work through the Canadian Organization for Rare Disorders, where he forged connections with those in the health-care space. He met computer scientist Michael Brudno from the University of Toronto, who, at the time, was the scientific director for SickKids’ Centre for Computational Medicine and co-founder of PhenoTips, a Toronto-based team that provides software and services to genetic health-care providers.
PhenoTips takes your genetic information and your list of symptoms and uses machine learning to search for other individuals with the same symptoms (phenotype) to then compare whether there are similarities in the related genomes (genotypes). The goal is to offer a potential differential diagnosis or to reveal a possible genetic marker for future research.
After hearing Stedman’s story at a conference, Brudno approached him and asked if he could digitize his medical records.
“He wanted to run my information through PhenoTips to see whether the software would be able to suggest a diagnosis,” says Stedman. “It took the software eight visits to figure out what was wrong with me … because he had a dataset of genomes that he could run it against, and so that was the moment where I thought, ‘OK, I’m not just doing law, I’m doing law and health policy now.’ ”
This experience inspired Stedman to pivot his professional focus and learn how to actualize this type of groundbreaking health-care tool for all Canadians.

“It took me 32 years to get a diagnosis, and it doesn’t seem like it has to be like that anymore. If I could enter the health-care system now, and if that system was allowed to learn from everyone’s health data, I could be diagnosed in one visit,” he says. “It’s actually my mission in life to figure out how that could be possible so that people like me – those coming up behind me – don’t have to tell a story like the one I tell.”
Drawn to the possibility of creating positive change in the health-care landscape, Stedman became more involved in advocacy work, learned more about health research, joined several boards related to rare diseases and genetics in medicine, and advanced his learnings as a social scientist in a new discipline.
Now, Stedman will lead a team responsible for patient partnership, participant engagement, training and outreach for the national genome database PCHGL.
Stedman emphasizes the significance of involving patients in scientific research and highlights the need for patient involvement, and education, in the PCGL initiative. This approach challenges the traditional health-care model and aims to enhance the role of patient partners.
The project provides an opportunity to empower patient partners in various aspects of the initiative and seeks to ensure their voices are heard in matters including technical decisions, ethics and policymaking.
Stedman will also contribute to a working group overseeing ethical and regulatory compliance for the library to meet its goal to collect, store and improve access to Canadian genomic data in a way that is equitable, secure and sustainable.
One of the key questions of the project is “How do we build a more inclusive genomic infrastructure in Canada?” says Stedman.
“Part of our project is to look at who is represented and who is not represented in the genomes we’ve sequenced in this country. With this library, we can start to take control over improving our representation within the data.”
Dr. Guillaume Bourque, director of the bioinformatics department at the McGill Genome Centre, will lead this initiative, collaborating with researchers from various partnering institutions. The database project is an extension of the Government of Canada’s Drugs for Rare Diseases Strategy. Its aim is to create a centralized genome library that reflects Canada's diverse population and empowers researchers and health-care professionals with invaluable insights.
“The real vision of this library is that it’s going to break down all the silos, so when someone gets diagnosed in Ontario, their doctor can say, ‘Let me go to the library and see what’s out there. Let me see who I can find, and whether they’ve consented to be contacted. Let me see if I can find other physicians who are affiliated with those genomes,’ ” says Stedman. “And it’s a lot easier, because it’s one massive registry.”
The library will be behind a secure infrastructure that allows researchers and medical professionals to access information, but not remove it. There are interdisciplinary experts in data infrastructure, ethics and governance, patient partnership and operating principles teaming up to realize this shared vision for this life-changing resource.
The team already has commitments from a few groups willing to share, with patient consent, genomic data. The hope is that within two years, PGCL will be close to launching.
“When you realize the power genomic data holds to help improve people’s health – and when you’ve lived that realization – it’s a lot easier to buy into the big idea,” says Stedman. “It’s visceral, it’s real. That’s what makes this project so powerful and that’s what I think will ultimately make this library successful.”
Stedman also serves on the executive of both the Centre for AI & Society and Connected Minds (CFREF) at York University.
